What is Interstitial Cystitis?
Interstitial cystitis is a bladder disease that causes chronic pelvic pain, a persistent and urgent need to urinate, and pain during sexual intercourse.
The symptoms of IC may appear in flares, with some people experiencing periods of relief in between, while others may have the symptoms constantly. The symptoms of IC can be similar to the symptoms of a urinary tract infection, but there is no evidence of bacteria or infection, and antibiotics do not help to relieve the pain. There is no difference in how IC affects men and women, but IC is much more common in women.
There is no cure for IC and treatment typically focuses on reducing symptoms like frequency, urgency, and pain. When the symptoms are reduced, IC patients can lead more comfortable lives.
IC sufferers often have to try different things to see what works for them. Different solutions work for different people and it is often necessary to try multiple methods before finding something that is effective. It’s also good to have a variety of possible remedies to try, as what works during one flare may not work during another.
Pathophysiology
There is no one universally accepted explanation for why patients develop IC, with various theories having been proposed to try and explain the condition’s pathophysiology. Though IC can be caused by a variety of things, most clinicians agree that things like a defective bladder lining, histamines released by mast cells, and autoimmune conditions are some of the main causes. Other situations, such as bladder trauma, bladder overdistention, pelvic-floor dysfunction, and spinal cord injury, can also contribute to IC. The following are descriptions of theories about IC pathophysiology.
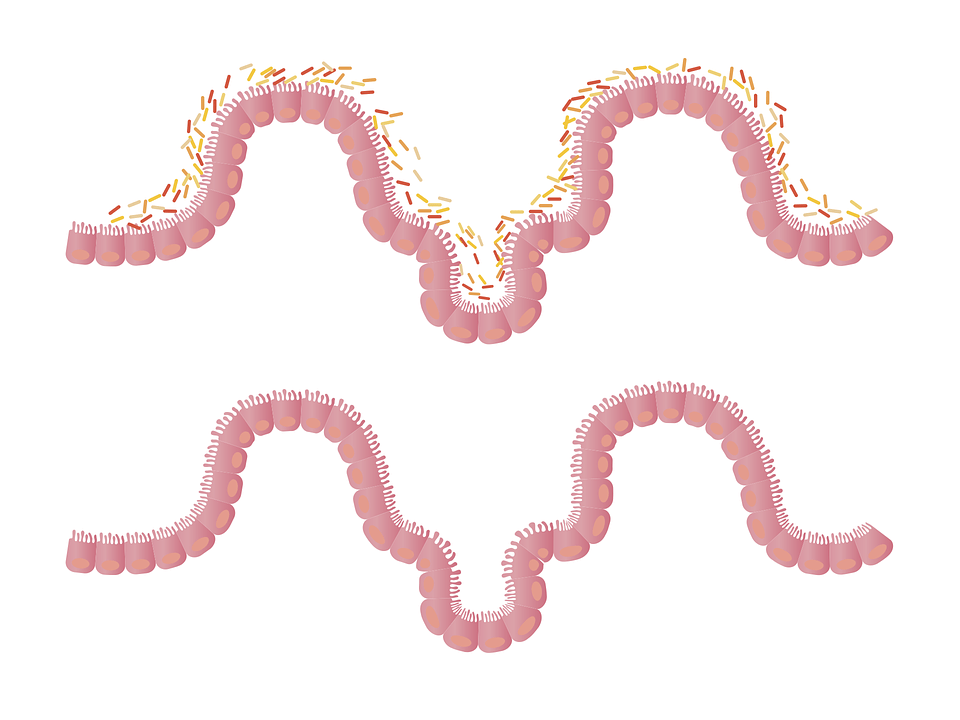
The most widely accepted theory is that a defect in the bladder lining allows waste in the urine (e.g., potassium ions) to infiltrate the nerves, causing pain and stimulating frequent urination. According to one study, the urine of IC patients had a lower potassium-to-creatinine ratio, which suggests that the permeability of the patients’ urinary systems is causing potassium to diffuse out of the body. This theory only explains 50% of IC cases because only 50% of IC patients had bladder-lining damage from petechial hemorrhage.
Mast cells are thought to play a role in the development of interstitial cystitis (IC). Recently, studies have found that mast cells containing histamine are involved in a variety of neural inflammatory diseases. If there is an irritation or infection of the bladder, or if it is stimulated by a chemical called acetylcholine, this will cause the mast cells to release a substance called histamine. The release of histamine causes smooth-muscle contraction, tissue damage, and nerve stimulation, which results in an inflammation response. Repeating these events may cause further damage to the bladder lining, resulting in a greater sense of urgency, frequency of bathroom trips, and pain. This theory does not explain all cases of IC, and using antihistamines to treat IC does not produce optimal results.
Some clinicians believe that immune-system dysregulation may play a role in the development of IC because some of the clinical features of IC resemble those seen in conditions characterized by a dysregulated immune system. IC also has links to autoimmune diseases and the pain syndrome connected to vulvar vestibulitis, fibromyalgia, Hashimoto’s thyroiditis, and irritable bowel syndrome, though the reasons for these associations are not clear. A study revealed that the majority of IC and endometriosis patients have chronic pelvic pain. The high percentage of chronic pain patients who also have IC indicates that a dysregulated immune system may contribute to IC.
Types of Interstitial Cystitis Flares
There are three primary types of interstitial cystitis flares: those involving the bladder wall, the pelvic floor muscles, and the muscles themselves.
Bladder wall flares are most often characterized by a feeling of something sharp scraping the inside of the bladder. During a flare, the bladder is often more inflamed than usual due to irritation from food or drink sensitivity.
Pelvic floor flares can be caused by sexual intercourse, long periods of sitting, or something as simple as riding a bike. The symptoms are more like a burning feeling in the urethra, vaginal area, or any part of the pelvic floor. The aforementioned conditions can also result in a sensation akin to something falling out of, or being pushed into, your vagina or urethra.
A muscle flare is when the muscle around the bladder goes into spasms. This can cause severe pain or aching in the bladder. The pelvic floor muscles may also become tight and cause pain.
Since traditional medical treatments haven’t been shown to provide much relief for IC patients in the long run, people with IC often seek out alternative methods to manage their chronic pain. Common therapies for treating GERD naturally are changing your diet, taking supplements such as marshmallow root or aloe vera pills, regulating your hormones, reducing stress, and increasing your water intake. You can also try physical therapies such as heat or cold therapy.
Signs and Symptoms
IC patients typically experience a strong urge to urinate immediately, as well as urinary frequency and bladder pain.3-6 The pain or spasms may or may not accompany the urge to urinate. Urinary urgency is strong, often sudden, urges to urinate. This leads to urinary frequency, with IC patients typically voiding many times per day. The average IC patient urinates up to 16 times per day, but the urinary volume is less than that of non-IC patients. Urinary urgency can often lead to the need to get up at night to urinate, which can then cause insomnia and fatigue.
In most cases, early-stage IC only involves one symptom, either urgency when urinating or going too often. However, eventually, bladder pain may develop and become a stronger symptom. Bladder pain may be felt in different areas, such as the suprapubic or perineal area, vagina, lower back, or medial aspect of the thigh. Because the pain is tough to identify the source of, the patient might think the pain is coming from a UTI.
Treatment
There are some principles that clinicians should follow to optimize treatment for IC. First, the goal is to alleviate or minimize symptoms. The most conservative treatment should be implemented first. The initial treatment should match the severity of the symptoms, be based on clinical judgment, and take into account the patient’s preferences. It is important to keep track of how well a person is doing before and after receiving multiple treatments as opposed to just one treatment. Unsuccessful treatments should be terminated after a clinically significant period has passed. It is important to consider how well pain is being managed and what effect it has on quality of life when making treatment decisions. If you don’t see any improvement in your symptoms after trying different treatments, you should go back and reconsider your diagnosis of IC.
The most conservative treatment option with the least risk of side effects should be initiated first, and then progress to less conservative options with a greater risk of side effects if necessary. The best possible scenario would be to minimize the risks of adverse drug reactions and maximize the benefits.
For treating IC in its early stages, the best course of action is to educate the patient on dietary and behavioral changes that can help manage the condition, as well as stress-relief techniques. As time goes on and the symptoms worsen, medication taken by mouth should be added.
There is only one type of medication that has been approved by the FDA for the treatment of IC, and that is pentosan polysulfate sodium (Elmiron). This drug works by adhering to the bladder wall mucosa to protect tissues from irritating substances in the urine. The recommended dosage is 100 mg taken orally three times daily, 2 hours before or after meals. ADRs that are most commonly reported include headaches, dizziness, alopecia, rashes, rectal hemorrhage, diarrhea, nausea, abdominal pain, and dyspepsia. The drug typically will not provide any symptom relief for at least 6 months. However, pain relief for early-phase IC patients may occur within 4 weeks. There is no data available on the risks and benefits of using this medication for longer than 6 months in patients who are unresponsive to treatment.
For patients with moderate-to-severe IC, a therapeutic regimen of Elmiron combined with antihistamines, antidepressants, and analgesics may be advised. Hydroxyzine hydrochloride can be used to help reduce IC symptoms for some patients. Specifically, a combination of pentosan and hydroxyzine has been shown to provide symptom relief in 40% of those who suffer from IC. Although hydroxyzine works similarly to an antihistamine, it comes with a range of potential side effects that may make it unsuitable for use with elderly patients. These potential side effects include central nervous system depression, itching, rashes, hives, dry mouth, tingling, tremors, and blurred vision.
Antidepressants like amitriptyline are often used to manage depression and pain in people with IC, as these patients are 3-4 times more likely to experience these issues. Amitriptyline relieves pain by inhibiting histamine secretion. Its reduction of norepinephrine and serotonin reuptake in the peripheral nervous system leads to less frequency and urgency. In a trial where people were randomly assigned to different groups, amitriptyline at a daily dose of 50 mg taken by mouth helped more than 50% of people with IC. The most common side effects are feeling tired, having a hard time going to the bathroom, and feeling like your mouth is dry.
Three types of pain medication that are often used to provide short-term relief during a flare-up of IC symptoms are phenazopyridine, nonsteroidal anti-inflammatory drugs, and narcotics.
Intravesical therapy involves injecting medication directly into the bladder. It can be used alone or together with oral medications for advanced IC, or when a patient doesn’t respond well to other conservative treatments or oral medications. An agent (usually DMSO) is used to reduce urgency, frequency, and pain by reducing inflammation, pain, and spasms. This method provides symptom relief at a dosage of 50 mL of 50% DMSO every 1 to 2 weeks for 4 to 8 weeks, but the pain frequently returns. In a study that randomizes and controls its participants, it was found that DMSO administered through the bladder wall was effective 70% of the time in reducing symptoms for a period of several months to a year. Heparin, which is also used for intravesical therapy, works by protecting the mucosal surface and reducing inflammation and scarring in the bladder. More than 50% of IC patients who received 25,000 U of heparin twice a week intravesically for 3 months showed significant improvement in symptom scores, according to one study.
If first- and second-line treatments do not work, then a cystoscopy with hydrodistention may be tried. The stretch stimulus from hydrodistention causes the heparin-binding epidermal growth factor to increase and antiproliferative-factor activity to decrease in the urine. This treatment provides a benefit of up to 6 months for 50% of IC patients. If Hunner’s lesions are found, a procedure using laser or electrocautery may be performed to destroy the lesions. The study found that all patients experienced complete pain relief, and 70% of patients also reduced or normalized their frequency levels for 2 to 42 months.
A surgically implanted neuromodulation device called InterStim is used to control urinary frequency and urgency in IC patients who fail conventional therapy. The FDA approved InterStim therapy in 1997 and it has been proven to be effective for up to 5 years. The device sends out electrical impulses through a thin wire connected to the sacral nerves. These nerves control the bladder, sphincter, and muscles on the pelvic floor. The device could be shut off at any moment, and the person would go back to the original condition. Patients who received InterStim therapy experienced a more significant improvement in quality of life than those who received standard treatments.
If past treatments haven’t worked to manage a person’s symptoms, cyclosporine A (CyA) may be an option to take orally. In a randomized trial, 75% of patients who were given oral CyA at a dose of 3 mg/kg/day showed significant clinical improvement after 6 months, compared to only 19% of patients who took Elmiron. Serious ADRs include immunosuppression and nephrotoxicity.
A cystectomy is a surgical procedure that involves removing all or part of the bladder. The procedure is not often used because it can be complicated and the results are not always predictable. It is only done in severe cases when other treatments have not worked. Supratrigonal cystectomy or urinary diversion may be used.
In supra trigonal cystectomy, a small portion of the bladder is removed and bowel tissue is used to form a new bladder. The procedure suggested increasing the size of the bladder, though it may affect the bladder’s regular emptying. This means that the patient has to put a tube into their bladder once or twice a day to empty it, which can cause infections. Additionally, the bowel produces mucus naturally, which may block the flow of urine or make self-catheterization more difficult.
In the urinary diversion, the flow of urine is redirected to a stoma (hole in the abdominal wall) by using a section of the bowel. The patient may choose to have the bladder removed entirely or to keep it and collect urine in an external bag that is attached to the stoma. This procedure has a lower risk of complications but the patient may find an external bag inconvenient. An alternative to an ileal reservoir is an internal pouch next to the abdominal wall. The pouch is made of tissue from the intestine and has a small stoma, or opening, where a catheter can be inserted to drain the pouch. Urinary diversion has a lot of complications and issues with mucus blockage.
Interstitial Cystitis Diet
One of the most popular methods for treating a urinary tract infection is to drink pure cranberry juice. This treatment can prove detrimental to IC sufferers. Cranberry juice is highly acidic and acidic foods are often known to irritate the bladder.
Common acidic bladder irritants include coffee, diet soda, alcohol, cranberry or other acidic fruit juices, tomatoes, chocolate, and lemons. An elimination diet allows people to figure out which foods, if any, make their flares worse.
Some IC sufferers take a product called Prelief when they know they will be eating an item that contains an acidic substance that can irritate the bladder.
Prelief contains calcium glycerophosphate, a dietary mineral that is a combination of calcium and phosphorus in a 1:1 ratio. The mineral can act as a base agent when added to acidic foods, which would neutralize the pH level of the food.
IC sufferers who follow an anti-inflammatory diet often find relief from their symptoms, as IC is an inflammatory disease. This diet is often wheat or gluten-free, and low in sugar, with few or no processed foods.